Research Summary
Research was conducted over multiple studies with various iterations of design and all done in South Africa. Below is a snapshot of the key numbers.

STUDIES
PARTICIPANTS
Research was conducted over multiple studies with various iterations of design and all done in South Africa. Below is a snapshot of the key numbers.

STUDIES
PARTICIPANTS
Insights are key synthesized learnings identified through the HCD approach. Each insight is supported by multiple research activities including behaviors, quotes, photos and other environmental observations. There are far too many insights to list here but below are a sample of key insights that guided the development of V in the South African context:

As a generation marked by scarcity, young people are willing to risk tomorrow for today.
The youth are experiencing unprecedented unemployment rates in South Africa, making it difficult to think about tomorrow as today is uncertain. So, people live for the moment. Women worry about immediate issues like finding work, moving to a better place or having enough money. Or they worry about pregnancy. They don’t worry about HIV infection because the consequences feel so far removed. In order to get immediate validation from their peer group through social media, they are willing to risk the consequences that may arise tomorrow for the status approval found today, even if it means getting involved with blessers and others means of transactional sex.

With men, the best approach is to say nothing. Or to reveal everything.
Every relationship is different with some men being more supportive than others. In general, however, when male partners receive just half the story about something newly introduced into the relationship (such as a partner using PrEP), they tend to assume the worst and act accordingly. For instance, an unfamiliar bottle is thought to be a muthi, spell or an indication that their partner has HIV. An old condom in a woman’s nightstand is a sign that she’s sleeping around. As such, it can be a good idea to either intentionally hide these items from more distrustful partners, or—if he’s of the kind that is likely to be supportive—disclose the entire story up-front.
Testing often requires an incentive or excuse.
While some are openly committed to regularly being tested so as to know their status, many require an excuse or an additional benefit in order to go through with it. People don’t like to admit they are at risk for HIV, so they need a different reason to tell their friends and partners why they went to the clinic. In the South Africa context, it’s “just for the Discovery Vitality points” is one reason. Or the test gets tacked on to another appointment or procedure, because “I was already there.”

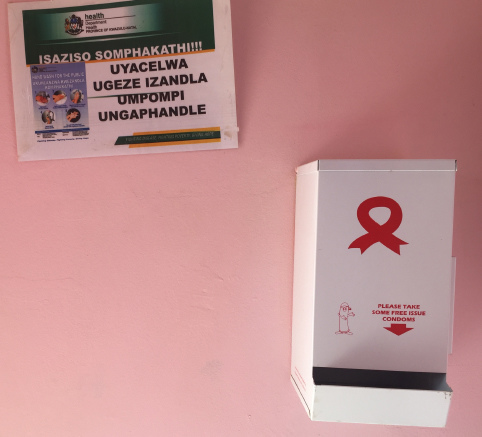
If it’s medical, you’re sick.
Pills and medical packaging are the markers of sickness, even if they are preventative. But people can think of prevention in a different way than treatment. The dosage form, the packaging, the messaging and the service surrounding them influences how people perceive prevention vs. treatment. Anything that reads as obviously medical will reinforce the assumption that the person with it is sick.

People are willing to go out of their way to visit private clinics and pharmacies where they can receive better service.
Even those who couldn’t truly afford to pay for medical care often made the investment. Furthermore, the shorter and quicker the journey the better. A long journey with multiple steps increases the effort and time required to get the product. It also has the potential to incur an additional cost of transport, which is just another barrier to potential use.
For more insights, please download this Research chapter:
Below are our Design Principles which provide a consistent experience across all interactions. These are actionable adaptations of our insights and are used as an internal tool to guide any design. No matter what you do as an intervention to increase uptake of and adherence to oral PrEP among young women, keep these principles in mind as you design it.

I want discretion, but that doesn’t mean I want boring. Bring me surprise and delight, especially in the face of something so dark as HIV.
For example:
Build in moments of delight and surprise throughout the PrEP experience to create excitement and encourage adherence through a prolonged engagement with the program or clinic providing PrEP.
Ensure that your design has no cues of anything medical (e.g., language, visuals).
Create moments throughout her experience with the product and brand that put the woman in control of whether to share her use of PrEP or to keep it secret.
Design products that have a sense of vibrancy and can blend in on a shelf with other products like makeup or perfume that women commonly use.

There’s so much to be skeptical of, especially when it comes to medical products. Help me get over my pessimism and give me something to trust enough that I give you my loyalty.
For example:
Use word-of-mouth marketing from trusted sources to drive awareness and build credibility of the brand/product.
Launch in private stores prior to distribution in government clinics to create a mental anchor point.
Create a big brand feel through media like TV, billboard, print, web and radio.
Ensure that any information is thorough, simple and non-judgmental.
Create packaging with common cues for legitimacy (for instance, high-quality materials).
Provide product feedback that helps women know it’s being used correctly.

HIV isn’t the first thing on my list—especially not today. Provoke me, get my attention through word-of-mouth, or give me tangible benefits for other priorities.
For example:
In South Africa, this means linking the brand to the concept of female empowerment—both on an individual basis and as a collective, as well as positioning the product as a woman’s product, like makeup or skincare.
Do not use the word “HIV”—it acts as a beacon which immediately turns people away.
Provide other benefits or rewards that motivate (both intrinsically and extrinsically).

Show me respect by giving me thoughtful options from which to choose. I want to protect myself, but it has to fit my life.
For example:
While only Oral PrEP is available, in the future it is recommended to provide multiple dosage forms with obviously differentiated use cases and users. Allow the women to self select so they have ownership over the dosage form they choose.
Throughout the journey, empower women with choice—whether or not they want to reveal their usage of the product, having a choice of tools to help adherence with the forms they can choose from and how they choose to spread the word.

Turn the HIV test into a moment to celebrate, with tools to help me stay negative. Instead of creating entirely new rituals, piggyback on behaviors that I already have.
For example:
Ensure that whatever you design is convenient—don’t make women work to get your product, or understand it, or use it.
Create a habit by linking the dosage to associated behaviors—such as getting ready in the morning or putting on makeup—and by using visual cues as a prompt.
Piggyback on other appointments and services to offer or advertise the HIV test and product.